Understanding Hysterectomy and Cancer Risk: What You Need to Know
The decision to undergo a hysterectomy is a significant one for women, often made in the context of various health issues, including fibroids, endometriosis, and cancer. However, one critical area of concern that frequently arises is the relationship between hysterectomy and cancer risk. In this article, we will explore how hysterectomy can impact cancer risk, the factors to consider, and the implications for women's health.
What is a Hysterectomy?
A hysterectomy is a surgical procedure that involves the removal of a woman's uterus. In some cases, the cervix, ovaries, and fallopian tubes may also be removed, leading to a total or radical hysterectomy. This surgery is typically performed to treat conditions such as:
- Uterine fibroids: Noncancerous growths that can cause pain and heavy bleeding.
- Endometriosis: A condition where uterine tissue grows outside the uterus, leading to chronic pain.
- Uterine prolapse: A condition where the uterus descends into the vaginal canal.
- Abnormal uterine bleeding: Unexplained heavy or irregular bleeding.
- Certain cancers: Such as uterine, ovarian, or cervical cancer.
Understanding Cancer Risks Associated with Hysterectomy
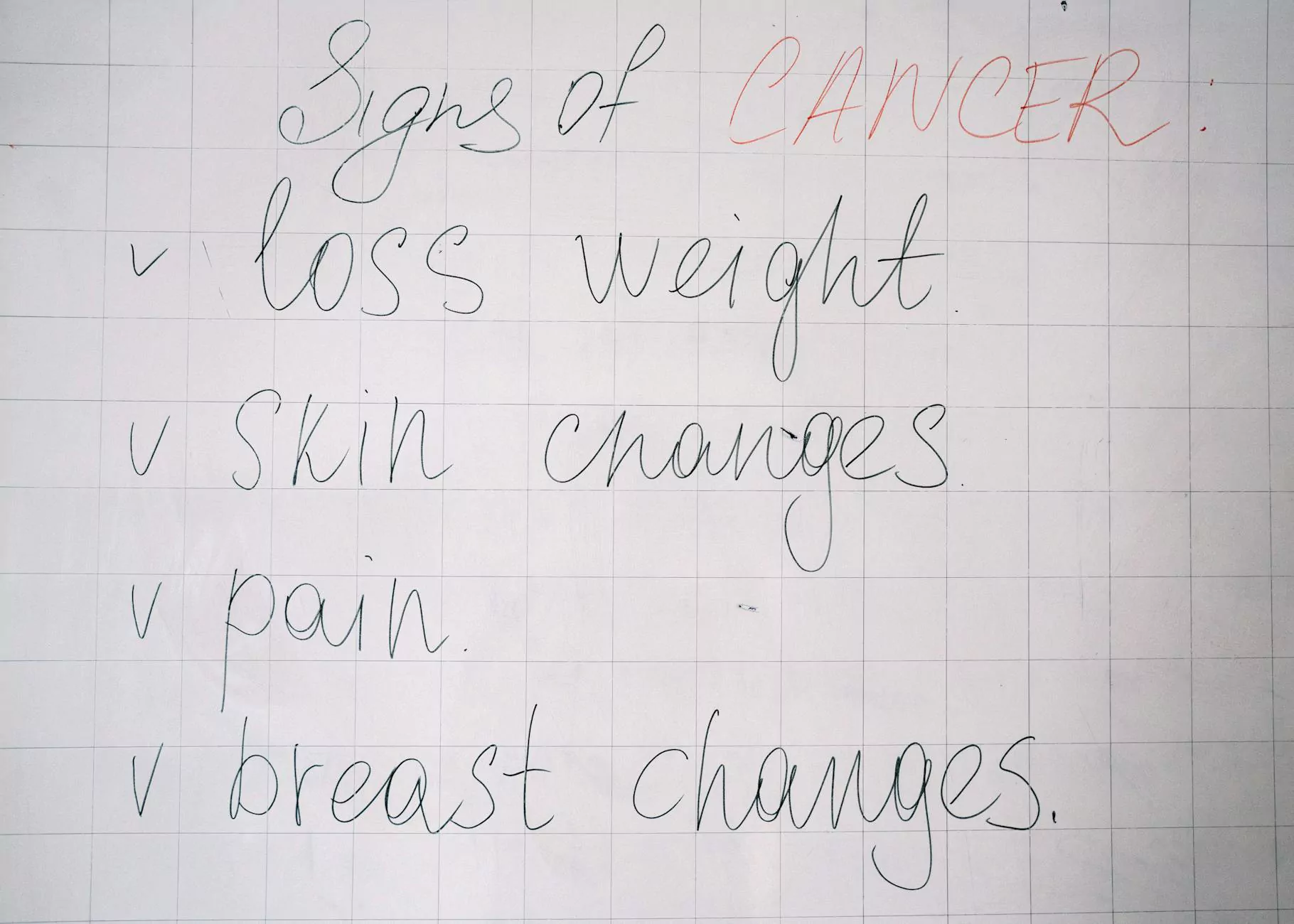
The relationship between hysterectomy and cancer risk is nuanced and depends on various factors. Let's delve into how a hysterectomy might influence cancer risks.
1. Hysterectomy and Uterine Cancer
Traditionally, one of the primary reasons for performing a hysterectomy is to manage or treat uterine cancer. For women diagnosed with this type of cancer, a hysterectomy may be a life-saving procedure as it removes cancerous tissue and can reduce the chance of cancer spreading.
2. Impact on Other Cancers
Research has shown that women who undergo a hysterectomy may experience changes in their risk for other types of cancers. Specifically:
- Ovarian Cancer: The removal of ovaries (oophorectomy) during a hysterectomy significantly lowers the risk of developing ovarian cancer.
- Cervical Cancer: Women who have undergone a total hysterectomy no longer have a cervix, thereby eliminating the risk of cervical cancer.
However, removal of ovarian tissue, while reducing certain risks, can also increase the risk of other health concerns, such as cardiovascular disease and osteoporosis.
Risk Factors to Consider
When discussing hysterectomy and cancer risk, it's essential to evaluate individual risk factors that may alter outcomes:
1. Family History
If there is a family history of reproductive cancers, it is essential to discuss these familial risks with your healthcare provider before undergoing a hysterectomy. Genetic predispositions can significantly influence cancer susceptibility.
2. Age and Menopause
The age at which a woman undergoes a hysterectomy can impact her health. For instance, women who have hysterectomies before the onset of natural menopause are at increased risk for conditions related to the sudden loss of estrogen.
3. Type of Hysterectomy
The type of hysterectomy performed (total, subtotal, radical) can also influence cancer risks post-surgery. A total hysterectomy may offer more comprehensive cancer risk reduction compared to a subtotal hysterectomy, which preserves the cervix.
Benefits of Hysterectomy Beyond Cancer Risk
While cancer risk is a critical component of the discussion surrounding hysterectomy, the procedure offers several other notable health benefits:
- Pain Relief: Many women experience significant relief from chronic pelvic pain and discomfort following a hysterectomy.
- Management of Heavy Periods: A hysterectomy can alleviate heavy menstrual bleeding, improving quality of life.
- Reduction of Specific Symptoms: Women with endometriosis or fibroids may find that a hysterectomy resolves debilitating symptoms that interfere with daily life.
- Elimination of Uterine Prolapse: For those suffering from prolapse, a hysterectomy can restore anatomical integrity and functionality.
Post-Hysterectomy Considerations
After a hysterectomy, it's crucial to keep several considerations in mind regarding long-term health and wellness:
1. Hormonal Changes
Women who undergo a hysterectomy, particularly younger women, may experience hormonal changes that can affect mood, energy levels, and overall health. Hormone replacement therapy (HRT) may be recommended to alleviate these symptoms.
2. Regular Health Screenings
Even after a hysterectomy, women should maintain regular health screenings for breast, kidney, and colorectal cancers, as the risk for these conditions remains unchanged.
3. Lifestyle Modifications
Adopting a healthy lifestyle, including regular exercise, a balanced diet, and avoiding smoking, can significantly enhance overall health and mitigate cancer risk. These lifestyle choices should be prioritized, especially after major surgeries such as a hysterectomy.
How to Navigate the Decision-Making Process
Deciding to undergo a hysterectomy is a deeply personal choice and should be approached with careful thought and discussion with healthcare providers. Here are some steps to guide the decision-making process:
- Consultation: Seek a thorough consultation with an experienced obstetrician/gynecologist to discuss the pros and cons of the surgery.
- Second Opinions: Don't hesitate to seek a second opinion, particularly if you're uncertain about the recommended procedure.
- Research: Educate yourself on all aspects of the procedure, potential risks, benefits, and recovery implications.
- Personal Reflection: Take time for personal reflection—consider your current health status, family history, and future health objectives.
Conclusion
Understanding the complex relationship between hysterectomy and cancer risk is vital for women considering this surgery. While a hysterectomy can significantly reduce the risk of various cancers, it is essential to be aware of the potential implications for overall health. It is crucial to approach this decision with comprehensive knowledge and support from medical professionals. For women exploring their options, resources such as drseckin.com provide valuable insights and expert guidance for navigating these important health decisions.
Empower yourself with knowledge, approach your healthcare team with questions, and make informed decisions about your reproductive health. Your well-being and peace of mind are worth it.









